Do patients with confirmed H. pylori Infection, who test negative for the CagA gene and are ulcer-free upon endoscopy, especially if there is no family history of stomach cancer, require antibiotics to clear their infection?
Based on 35 years of practice and study (I published the internet’s first protocol on H. pylori treatment back in 2009), I will share some thoughts to consider. This is not an in-depth review but more of a flowchart to help you make a more informed choice.
Personally, I don’t recommend antibiotics as a first-line option. Non-invasive options should be used first to see if the current symptomatology can be resolved. I have helped many patients in this situation, who were convinced that antibiotics were the only option, resolve their symptoms and get back to a more normal life.
Table of Contents
- A. Introduction
- Understanding H. pylori Infection
- Overview of H. pylori
- Importance of cytotoxin-associated gene A (CagA)
- C. Diagnosis: Positive for H. pylori, CagA Negative, and No Ulcer Detected
- Significance of CagA Status
- Endoscopy Findings
- Treatment Approaches
- Antibiotics and H. pylori Eradication
- Importance of Tailored Treatment Plans
- Lifestyle Modifications
- The Debate on Antibiotics
- Risks and Benefits
- Monitoring H. pylori Infections
- Shared Decision-Making with Healthcare Providers
- Natural Remedies and Adjunct Therapies
- Probiotics
- Dietary Changes
- Herbal Supplements
- Conclusion
- FAQ
Introduction
Helicobacter pylori is a spiral-shaped bacterium that colonizes the stomach lining, and its infection is a global health concern. When patients receive a positive diagnosis for H. pylori but test negative for CagAI and show no ulcers during endoscopy, especially if there is no family history of gastric cancer, the optimal course of action becomes a subject of consideration.
Understanding H. pylori Infection
Overview of H. pylori
H. pylori is a common bacterium that often infects the stomach during childhood. While many infections remain asymptomatic, some cases can lead to gastritis, peptic ulcers, and, in rare instances, gastric cancer.
Importance of cytotoxin-associated gene A (CagA)
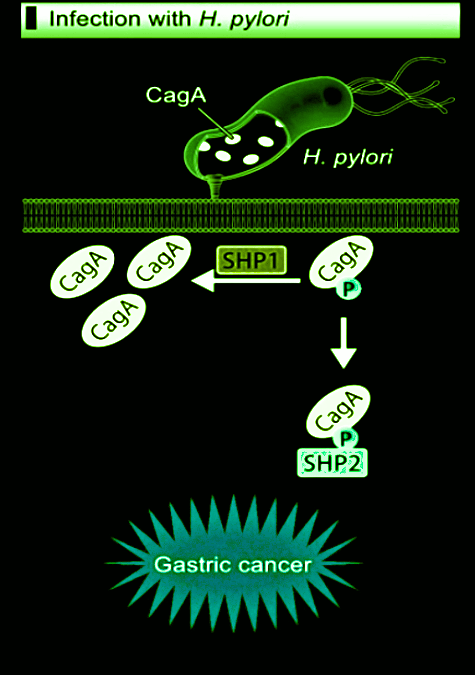
CagA is one of the most studied pathogenicity factors of the bacterial pathogen Helicobacter pylori. Chronic infection with Helicobacter pylori CagA-positive strains is the strongest risk factor for gastric cancer. Its presence is associated with increased virulence and a higher risk of severe clinical outcomes.
Diagnosis: Positive for H. pylori, CagA Negative, and No Ulcer Detected
Significance of CagA Status
Patients testing positive for H. pylori but negative for CagA may experience a milder disease course. The absence of ulcers during endoscopy further complicates the decision of whether to treat or not. The diagnosis of H. pylori does not guarantee that your symptoms were caused by it, especially without the presence of virulence factors and ulcer.
Endoscopy Findings
Endoscopy is a crucial diagnostic tool, allowing healthcare providers to visualize the stomach lining. When no ulcers are detected, the focus shifts to managing the infection, symptomatology, and preventing complications.
Treatment Approaches
Antibiotics and H. pylori Eradication
Antibiotics have traditionally been the cornerstone of H. pylori treatment. However, the necessity of antibiotics in cases without CagA and no ulcers is a subject of ongoing debate. Do the benefits outweigh the potential for an unwanted outcome, as well as the potential for the original symptoms to be unresolved?
Importance of Tailored Treatment Plans
Individualized treatment plans, considering the patient’s overall health, risk factors, and preferences, are pivotal in achieving successful outcomes. (714-639-4360 to book your complimentary 15-minute consultation to see if we are a good fit.
Lifestyle Modifications
In addition to antibiotic therapy, lifestyle changes, including dietary adjustments and stress management, can contribute to better outcomes.
The Debate on Antibiotics
Risks and Benefits
Antibiotics, while fairly effective against H. pylori, may pose risks such as antibiotic resistance and unwanted side effects. The decision to prescribe antibiotics should weigh all negative factors against potential benefits. Additional Information.
Monitoring H. pylori Infections
Regular follow-up and monitoring of H. pylori infections help healthcare providers assess the effectiveness of treatment and adjust plans as needed. Diagnostic Testing may include Diagnostic Solutions’ (GI-MAP | GI Microbial Assay Plus w/ H. pylori Antigen and Virulence Factors – $425) as well as stand-alone H. pylori stool antigen testing.
Shared Decision-Making with Healthcare Providers
Collaborative decision-making between patients and healthcare providers ensures that treatment plans align with individual preferences and values.
Natural Remedies and Adjunct Therapies
Probiotics
Probiotics show promise in managing H. pylori infections by promoting a healthy gut microbiota. Research suggests a potential role in reducing H. pylori-associated symptoms – Pylopass Eliminates H. pylori with Confidence.
Dietary Changes
Certain dietary modifications, such as incorporating antioxidant-rich foods (polyphenols), may complement treatment efforts and support overall gastric health.
Herbal Supplements
Some herbal supplements, including mastic gum and licorice root, have been explored for their potential antimicrobial properties against H. pylori.
Conclusion
In conclusion, the decision to prescribe antibiotics for patients with confirmed H. pylori infection, CagA negative, and no ulcers detected involves careful consideration of various factors. While antibiotics remain a standard treatment, individualized plans incorporating lifestyle modifications and potential natural remedies should be explored. Shared decision-making between patients and healthcare providers is paramount to achieving optimal outcomes.
FAQ – CagA and H. pylori
Q1: Is H. pylori infection common?
Yes, H. pylori infection is widespread and affects a significant portion of the global population.
Q2: What is the significance of CagA in H. pylori infections?
CagA is associated with increased virulence, leading to more severe clinical outcomes, such as gastric cancer.
Q3: How is H. pylori infection diagnosed?
Diagnosis typically involves tests such as breath tests, blood tests, and endoscopy.
Q4: What does it mean to be CagA negative?
Being CagA negative suggests a potentially milder disease course.
Q5: Can H. pylori infections cause ulcers?
Yes, H. pylori infections are a major cause of peptic ulcers.
Q6: Are antibiotics the only treatment for H. pylori infections?
While antibiotics are common, individualized treatment plans may include other approaches.
Q7: How does endoscopy help in the diagnosis of H. pylori infections?
Endoscopy allows visualization of the stomach lining to detect ulcers and assess the severity of infection.
Q8: What lifestyle changes can help manage H. pylori infections?
Lifestyle changes include dietary modifications, stress management, and avoiding certain triggers.
Q9: Are there risks associated with antibiotic treatment for H. pylori?
Yes, risks include antibiotic resistance and potential side effects.
Q10: Can H. pylori infections be monitored over time?
Yes, regular follow-up allows healthcare providers to assess the effectiveness of treatment.
Q11: Do natural remedies like probiotics have a role in H. pylori management?
Research suggests that probiotics may support overall gastric health and reduce symptoms.
Q12: Is collaborative decision-making important in H. pylori treatment?
Yes, shared decision-making ensures that treatment plans align with individual preferences and values.