Gut-Brain Axis Image – © 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
I read Uncovering the Mysteries of the Gut-Brain Connection by Helen Albert, and it was everything I was looking for: a thorough, thoughtful article that covers critical insights into the topic with facts from the researchers on the front lines doing the work. And it’s this work that, hopefully, will lead to better understanding and cures for various neurological diseases and conditions. I rewrote this with some additional information to help me better understand all that was said, and I’m sharing my version here. This is with grateful acknowledgment to the original article and author, Helen Albert.
Table of Contents
- Introduction to the Gut-Brain Axis
- The Microbiome: A Key Player in the Gut-Brain Axis
- Neurological Disorders Linked to the Gut-Brain Axis
- Parkinson’s Disease and the Gut
- ALS and Gut Microbiome Research
- Autism Spectrum Disorder and the Microbiome
- Probiotics and the Future of Mental Health
- Diet, the Microbiome, and Brain Cancer
- Challenges and Future Directions
- Conclusion on the Gut-Brain Axis
Introduction to the Gut-Brain Axis
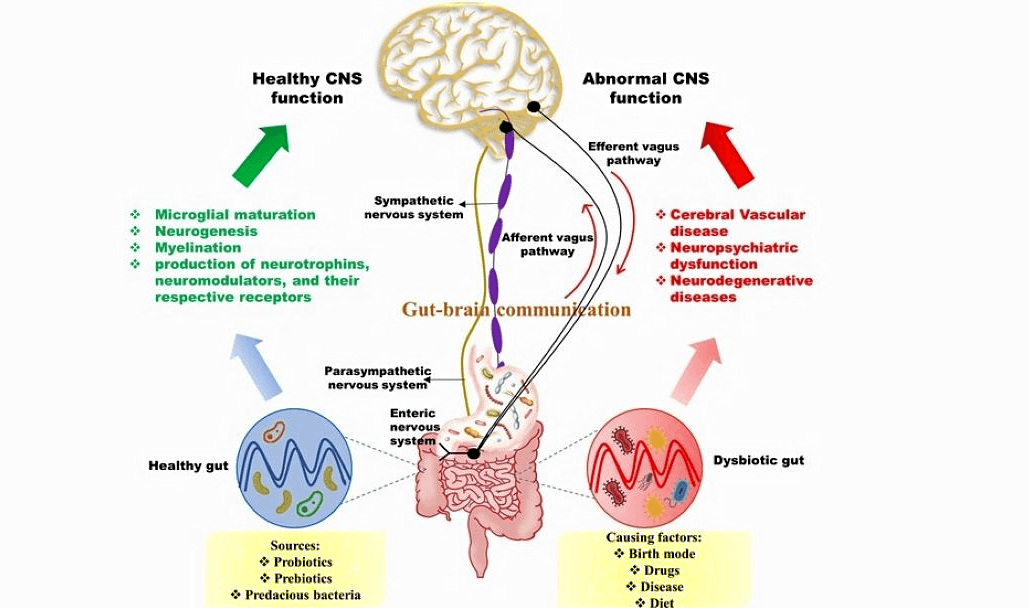
For decades, scientists have understood that there is a complex and vital connection between the gut and the brain. This relationship, commonly called the “gut-brain axis,” involves a bi-directional communication system where the gut and brain share information through various pathways. However, over the last 20 years, researchers have uncovered the pivotal role that the gut microbiome—the trillions of microorganisms living in our digestive system—plays in this interaction. From influencing emotional states and digestion to impacting neurological health, the gut microbiome is proving to be a key player in understanding and potentially treating various brain disorders.
The concept of the gut-brain connection was first proposed in the 19th century. In the 1840s, U.S. Army surgeon William Beaumont observed that emotional states could directly affect digestion. This early observation laid the foundation for a communication system between the gut and the brain. In 1904, Nobel laureate Ivan Pavlov further illustrated this connection through his famous experiments, demonstrating that external stimuli could influence digestive processes.
The “gut-brain axis” has now evolved into a broader scientific exploration. Researchers are studying how these two systems communicate and how the gut microbiome influences neurological function.
The Microbiome: A Key Player in the Gut-Brain Axis
The gut-brain axis operates through three main channels: immune cells, soluble molecules, and neurological pathways. The gut houses around 168 million nerve cells, making it so neurologically dense that it is sometimes called the “second brain.” The vagus nerve, one of the longest nerves in the body, links the brain directly to the gut, facilitating continuous communication between the two systems.
The gut microbiome has become a focal point of research in this area. According to John Cryan, PhD, a leading researcher at University College Cork, the microbiome is critical in regulating the gut-brain axis. Gut microbes produce chemicals such as neurotransmitters, hormones, and metabolites that can either protect or disrupt brain function, influencing behavior and neurological health. These chemicals can enter the bloodstream, interact with immune cells, and even influence the blood-brain barrier, making the gut microbiome essential in maintaining neurological balance.
Neurological Disorders Linked to the Gut-Brain Axis
Emerging research increasingly points to the microbiome as a significant factor in the development of various neurological conditions. Studies have drawn links between gut health and disorders such as attention-deficit hyperactivity disorder (ADHD), Parkinson’s disease, autism, amyotrophic lateral sclerosis (ALS), and more. Although much of the early research has been conducted in animal models, researchers are optimistic that these findings can be translated to humans as trials progress.
Parkinson’s Disease and the Gut
Parkinson’s disease is a neurodegenerative disorder characterized by the accumulation of a protein called alpha-synuclein in the brain, leading to a progressive loss of motor control. Intriguingly, English surgeon James Parkinson first described gastrointestinal (GI) dysfunction as a symptom of Parkinson’s disease in his 1817 treatise on the disease. Parkinson’s noted that patients with the condition, which he called “shaking palsy,” often experienced constipation. In one case, treating the patient’s GI issues improved their movement problems.
Recent research by Sarkis Mazmanian, PhD, at the California Institute of Technology, supports this hypothesis. His team has found that over-colonization of the gut with Escherichia coli-like bacteria, which produce bacterial amyloid called curli, may lead to alpha-synuclein accumulation in the gut and the brain. This accumulation has been shown to cause both motor and gastrointestinal symptoms in animal models, mimicking those seen in Parkinson’s patients. Mazmanian’s ongoing research suggests that the vagus nerve may be involved in transmitting these pathological signals from the gut to the brain.
ALS and Gut Microbiome Research
ALS, or amyotrophic lateral sclerosis, is another neurodegenerative disease that researchers are now linking to gut health. ALS leads to the deterioration of motor neurons, and while genetic factors play a role, environmental factors, including gut dysbiosis, are also implicated. In both animal models and human patients, abnormalities in the gut microbiome are often present before the onset of symptoms.
French biotech company MaaT Pharma is currently testing a novel gut microbiome-based treatment for ALS. The therapy, MaaT033, involves fecal microbiota transplantation into the guts of ALS patients to reduce inflammation and stabilize the gut environment. Initial trials have been promising, and researchers hope to have more definitive results by the end of the year.
Autism Spectrum Disorder and the Microbiome
Research is also uncovering the microbiome’s role in autism spectrum disorder (ASD). People with autism frequently experience gastrointestinal issues, and scientists have found that these individuals often have lower levels of the beneficial bacterium Bacteroides fragilis. Sarkis Mazmanian and his team discovered that mice with autism-like behaviors had elevated levels of a compound called 4-ethylphenylsulfate produced by gut bacteria. Remarkably, when these mice were supplemented with Bacteroides fragilis, their behavior and gut health improved significantly.
Mazmanian’s research has led to the founding of Axial Therapeutics; a company focused on developing microbiome-based treatments for conditions like autism and Parkinson’s. One of their lead candidates is AB-2004, currently in Phase II trials. Scientific research suggests a possible connection between bacteria in the digestive system and the brain, which may influence specific behaviors like anxiety and irritability. AB-2004 is under investigation as a potential new treatment aimed at managing irritability in children with ASD. This compound is formulated to bind (sequester) certain gut-bacteria-derived substances, reducing their chances of entering the bloodstream and affecting the brain.
Probiotics and the Future of Mental Health
The gut microbiome’s influence on mental health is not limited to neurodevelopmental and neurodegenerative diseases. Probiotic supplementation is emerging as a potential tool for maintaining mental well-being, particularly in aging populations. Julia Rode, PhD, a researcher at Örebro University in Sweden, is currently studying whether probiotic use can help preserve cognitive function as people age. Her work is focused on evaluating the impact of probiotics on compromised populations, such as those experiencing early signs of cognitive decline.
Diet, the Microbiome, and Brain Cancer
Diet also appears to play a role in the gut-brain axis, particularly in conditions such as brain cancer. Although research in this area is still in its infancy, Khalid Shah, PhD, a professor at Harvard University, believes that dietary interventions, such as the ketogenic diet, could complement conventional treatments like chemotherapy. Shah points out that many brain cancer patients on ketogenic diets report fewer side effects from chemotherapy and generally feel better, which could be linked to the gut-brain connection.
Challenges and Future Directions
While the connection between the gut microbiome and neurological health is increasingly clear, the field still faces several challenges. One of the biggest hurdles is the heterogeneity of studies. Researchers like Arias Vásquez note that inconsistencies in study designs and bioinformatics pipelines make replicating findings and drawing firm conclusions difficult. More standardized and rigorous research is needed before microbiome-based therapies can be widely approved.
Despite these challenges, the field is moving forward. In 2022, the first microbiome-based therapies were approved to treat recurrent Clostridium difficile infections, a significant milestone for the field. Although no such treatments for neurological diseases have yet been approved, many are in the early stages of clinical trials.
Looking to the future, John Cryan envisions a time when people can monitor their microbiome in real-time, linking changes in gut health to mental and neurological well-being. This could be particularly important for maintaining cognitive function and mental health as people age.
Conclusion on the Gut-Brain Axis
The gut-brain axis and the role of the microbiome in neurological health represent one of the most exciting areas of modern scientific research. While much remains to be discovered, the potential for new treatments targeting the microbiome is vast. From Parkinson’s disease and ALS to autism and mental health, the gut microbiome holds the key to understanding—and potentially treating—many of the most challenging neurological conditions. As research progresses, integrating microbiome-based therapies into mainstream medicine could revolutionize how we approach brain health in the years to come.
Similar Topics
Protein Digestion and SIBO
Threonine-Rich Foods Boost Gut Health: Akkermansia & Faecalibacterium
Artificial Light at Night Causes Anxiety, PTSD, Bipolar Disorder
Metabolic Programming Importance Early In Life